Цена на дизельное топливо и нефтепродукты: влияние на мировую экономику и потребителей
Введение Нефтепродукты являются одним из основных источников энергии в мире и используются в широком спектре отраслей, включая транспорт, производство и сельское хозяйство. Одним из наиболее популярных нефтепродуктов является дизельное топливо,…
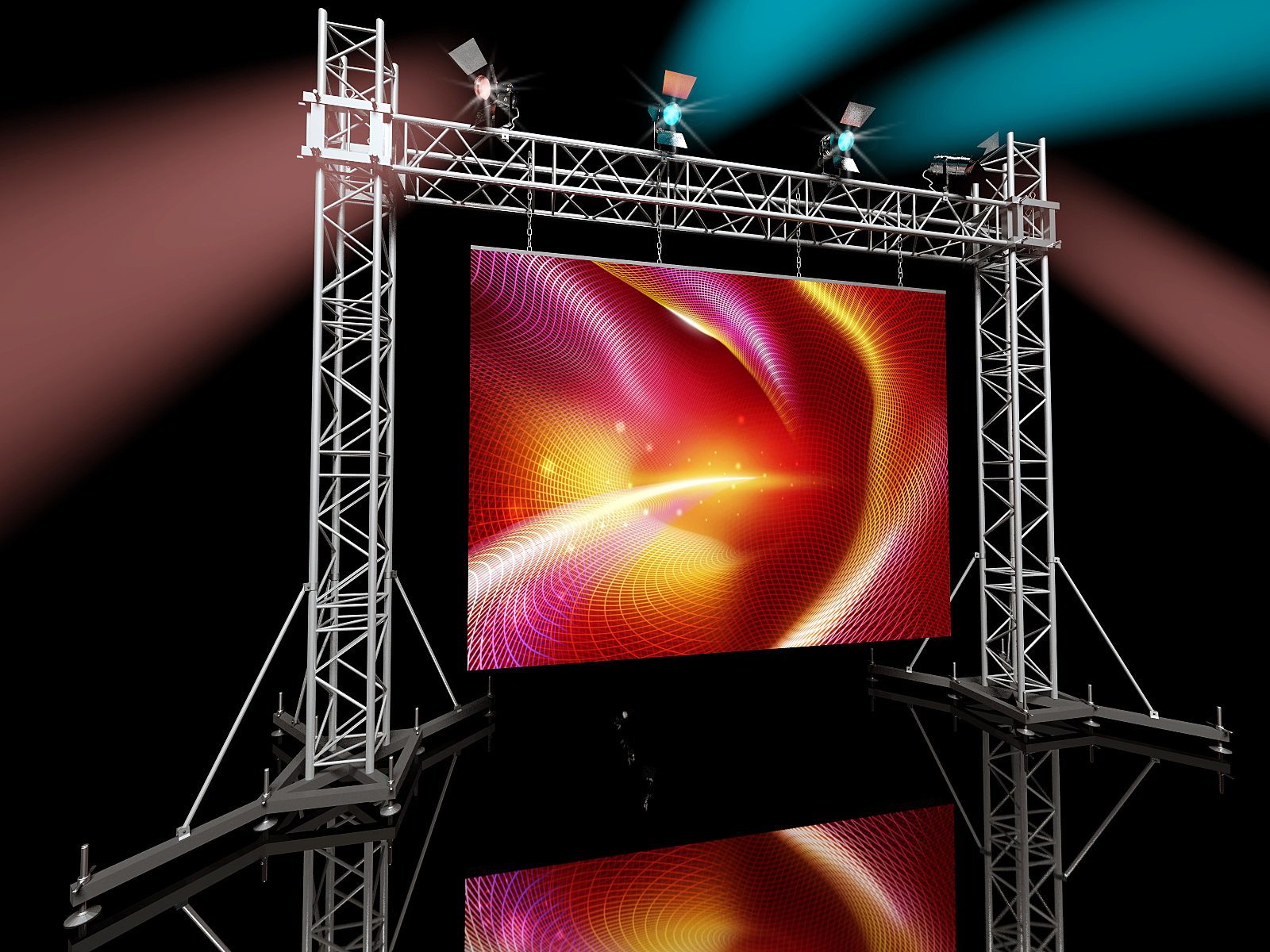
Аренда светодиодного экрана: как выбрать и где использовать
Введение Современные технологии в области дисплеев и проекций позволяют создавать невероятные визуальные эффекты и привлекать внимание аудитории. Среди них особое место занимают светодиодные экраны — устройства, которые позволяют показывать яркие…
Зачем организациям нужен ИТ-аутсорсинг и как выбрать подходящего провайдера
Введение ИТ-аутсорсинг – это процесс передачи управления и обслуживания сетей и информационных технологий (ИТ) третьей стороне. Эта модель становится все более популярной среди компаний, желающих сосредоточить свои усилия на основном…
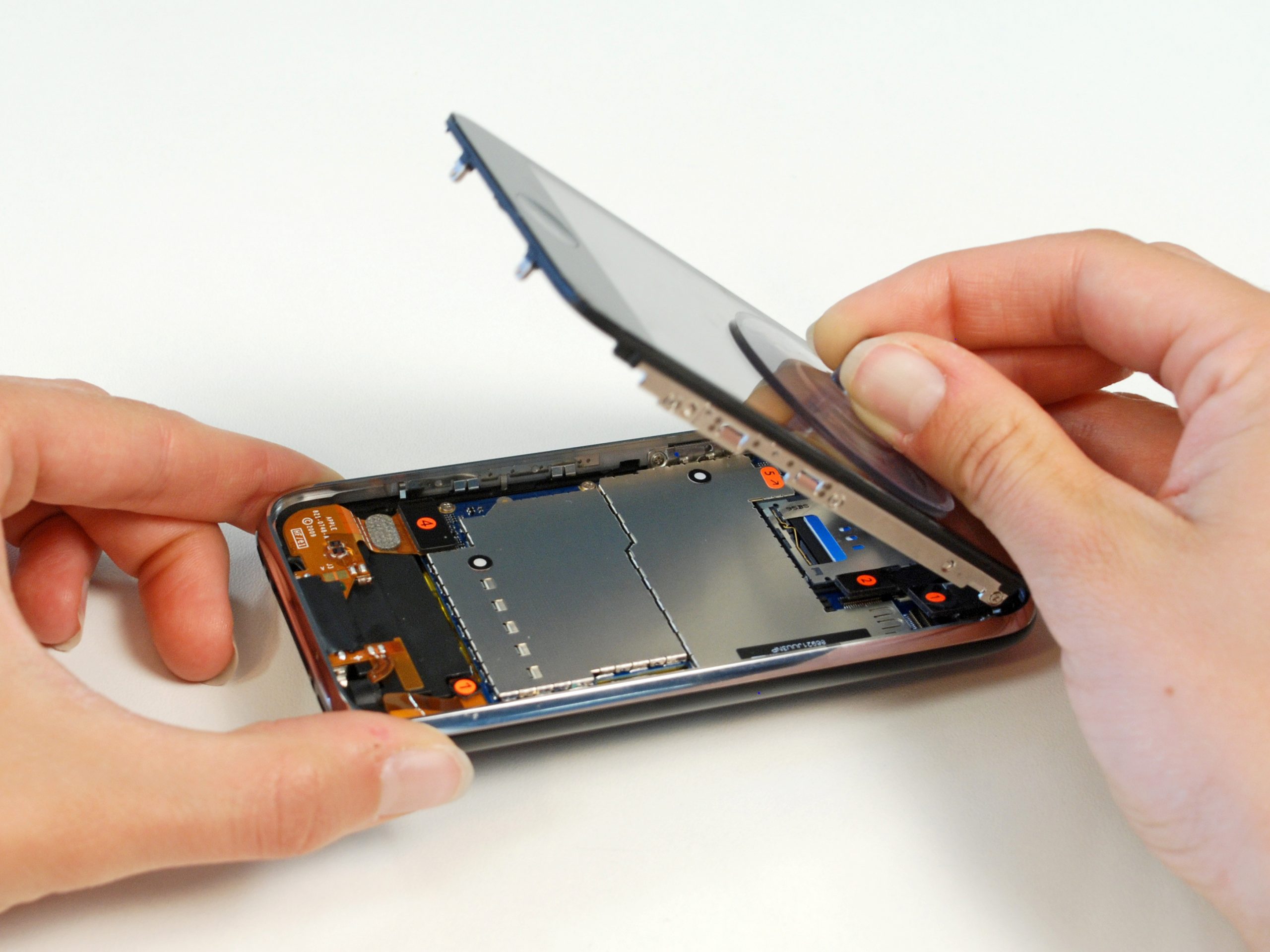
Современные технологии и сложность ремонта
Вступление С появлением новой модели iPhone 14, многие владельцы старых устройств задумываются о возможности выполнения ремонта своих гаджетов. В этой статье мы рассмотрим основные аспекты ремонта iPhone 14 и дадим…
DIGITAL-АГЕНТСТВО: Как оно может помочь вашему бизнесу
Введение В современном мире, где все больше и больше людей проводят свое время в онлайн пространстве, важно иметь сильное присутствие в сети для успешного бизнеса. Именно поэтому все больше компаний…
Системный digital-маркетинг
Введение В современном мире, где все больше и больше людей предпочитают делать покупки онлайн, digital-маркетинг становится неотъемлемой частью успешного бизнеса. Он позволяет привлекать новых клиентов и увеличивать продажи, используя различные…
Восстановление жесткого диска
Введение Восстановление жесткого диска – это процесс, который позволяет восстановить работоспособность данного устройства после различных повреждений. Жесткий диск является одним из самых важных компонентов компьютера, так как хранит на себе…
Обслуживание серверов: основные аспекты и рекомендации
Введение Серверы – это центральные устройства в компьютерной сети, которые обеспечивают обмен информацией и хранение данных. Правильное и своевременное обслуживание серверов является важной частью управления IT-инфраструктурой любого предприятия. В данной…
Города мира: многообразие культур и архитектуры
Введение В мире существует огромное количество городов, каждый из которых обладает своей уникальной историей, культурой и архитектурой. От маленьких провинциальных городков до огромных мегаполисов, каждый город имеет свой неповторимый характер…
Продвижение сайтов для роста продаж: эффективные стратегии и методы
Введение В современном мире интернет-технологии занимают все более важное место в бизнесе. Для многих компаний сайт стал не только визитной карточкой, но и основным инструментом для привлечения новых клиентов и…